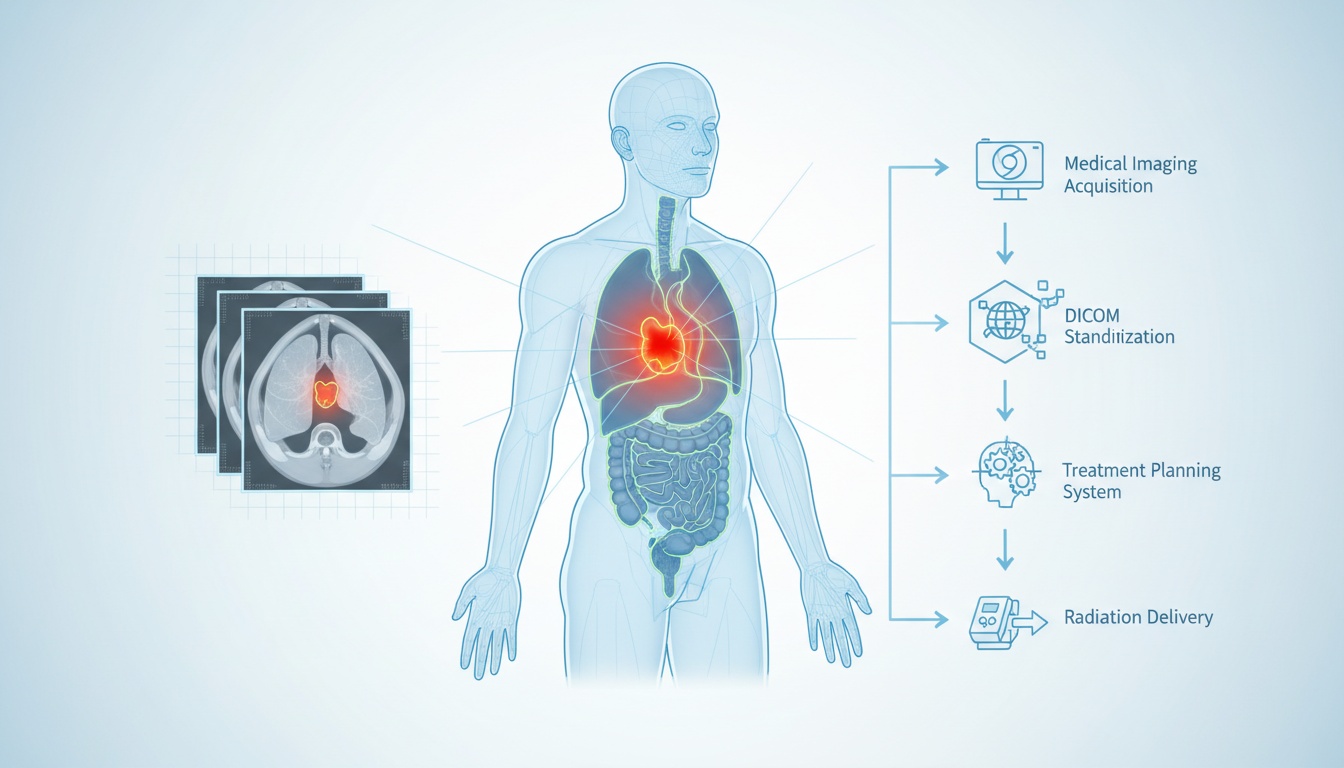
Radiation therapy is one of the most effective tools in the fight against cancer. It relies on the precise delivery of high-energy radiation to shrink or destroy tumors while sparing healthy surrounding tissues. But the key word here is precision. Without pinpoint accuracy, radiation therapy risks harming vital structures or failing to target malignant cells effectively. That level of precision doesn’t happen by accident—it begins with imaging.
Medical imaging is the backbone of radiation therapy planning. It allows radiation oncologists and medical physicists to visualize the tumor, surrounding organs, and tissue densities to tailor a unique treatment plan to each patient. This is where DICOM (Digital Imaging and Communications in Medicine) comes into play. DICOM images standardize how scans are captured, stored, transferred, and viewed, ensuring consistency across devices and systems.
In this article, we’ll explain how imaging supports radiotherapy planning, how DICOM images work in this context, and how radiation mapping ensures safe, effective treatment. Whether you're a student, medical professional, or someone exploring radiology platforms, you'll gain a deeper understanding of how pictures of radiation therapy translate into successful outcomes.
The imaging process is foundational to radiotherapy. Before any beams are directed at the body, clinicians must locate the tumor and identify nearby healthy tissues needing protection. This is done through a simulation session, typically involving a CT scan, which creates a detailed 3D model of the patient’s anatomy.
CT scans are considered the gold standard for radiation therapy planning due to their excellent spatial resolution and ability to quantify tissue density. MRI is often used alongside CT for better visualization of soft tissues, especially in brain, spinal cord, or pelvis cases. PET scans may also be incorporated to highlight metabolically active regions within a tumor, offering additional insights into tumor biology.
These imaging modalities generate cross-sectional slices of the body that, when compiled, form a comprehensive anatomical map. These maps help clinicians identify the Gross Tumor Volume (GTV), Clinical Target Volume (CTV), and Planning Target Volume (PTV), each of which represents a crucial component in defining where and how the radiation will be delivered.
When patients look for pictures of radiation therapy, they often want to understand what the machines look like or what the process entails. However, the more critical images are the ones captured internally—the diagnostic and planning scans that allow for precise and safe treatment.
DICOM is a universal format used to handle, store, print, and transmit information in medical imaging. It encompasses both a file format and a communication protocol. Introduced in the early 1990s, DICOM has become the industry standard for radiological imaging and is widely adopted in hospitals and clinics worldwide.
In the context of radiation therapy, DICOM goes beyond just storing CT or MRI images. It includes specialized extensions known as DICOM RT objects. These include:
• Rtstruct: Defines the structure sets, such as tumors and organs at risk.
• Rtplan: Contains the technical details of how radiation will be delivered.
• Rtdose: Holds the calculated dose distribution across the treatment area.
• Rtimage: Captures verification images taken during treatment.
DICOM images allow multiple systems—scanners, treatment planning software, and radiation delivery machines—to communicate seamlessly. A scan taken on a CT machine can be transferred to planning software where contours are drawn, dose calculations are performed, and the finalized plan is exported to a linear accelerator for delivery.
These images and related metadata ensure that the patient receives the correct dose, to the correct area, with millimeter-level accuracy. They also allow for archiving and reviewing of treatment data, which is crucial for quality assurance and long-term follow-up.
The radiation therapy planning process is a highly coordinated sequence of steps involving radiologists, radiation oncologists, medical physicists, and dosimetrists. It begins with the simulation phase. During this phase, the patient is positioned exactly as they will be during actual treatment, and immobilization devices may be used to ensure reproducibility. A CT scan is then performed in this setup.
Once the scan is acquired, it is saved in DICOM format and imported into treatment planning software. Here, the medical team identifies and outlines the tumor and adjacent organs at risk. This step is known as contouring, and it is critically important. Even a few millimeters off can mean the difference between targeting the tumor effectively or damaging healthy tissue.
With structures defined, the medical physicist or dosimetrist begins dose planning. The goal is to maximize the radiation dose to the tumor while minimizing exposure to normal tissues. Advanced algorithms calculate the optimal arrangement of radiation beams to achieve this balance. These parameters are then saved as a DICOM RTPLAN.
The calculated dose distribution is stored as a DICOM RTDOSE file, which provides a 3D map showing how radiation will be deposited throughout the body. The radiation oncologist reviews and approves this information before it is sent to the treatment machine.
DICOM RTIMAGE files may be generated during actual treatment to verify patient positioning and ensure that radiation is being delivered as planned. This verification step is crucial for maintaining treatment accuracy over multiple sessions.
Radiation mapping refers to visualizing how radiation dose is distributed within the patient’s body. This is critical in ensuring the prescribed dose reaches the tumor while limiting exposure to surrounding tissues.
Treatment planning systems can simulate how radiation will behave as it passes through different tissues using data from CT and MRI scans. These simulations account for the physical properties of the radiation beam and the patient’s anatomy.
The result is a 3D dose distribution, often visualized through color-coded isodose lines. These lines represent areas receiving specific percentages of the prescribed dose. For example, the 100% isodose line should ideally encompass the tumor volume, while lower percentages might spread into adjacent areas.
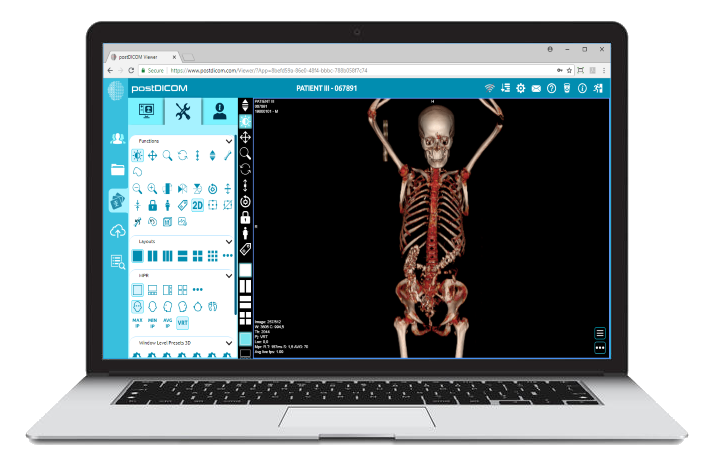
DICOM RTDOSE files contain this mapping information. When viewed in a DICOM viewer like PostDICOM, clinicians can examine each slice, rotate the model, and evaluate dose coverage from multiple angles. This ensures that the treatment plan meets clinical objectives before it is executed.
Pictures of radiation therapy often focus on machines or treatment rooms, but radiation mapping offers a more profound picture—one that shows the invisible lines guiding life-saving treatment.
 - Created by PostDICOM.jpg)
The use of DICOM in radiotherapy brings numerous advantages that directly impact patient safety, treatment effectiveness, and operational efficiency.
First and foremost, DICOM ensures interoperability. Regardless of which scanner is used or which planning software is implemented, as long as all systems support DICOM, the data can flow seamlessly. This enables institutions to mix and match equipment without compromising workflow integrity.
Secondly, DICOM allows for standardized documentation and storage. Treatment plans, images, and dose maps can be archived for future reference, allowing clinicians to review and compare past therapies if cancer recurs. This historical data is invaluable in long-term cancer management.
Moreover, DICOM-based systems enable remote collaboration. A radiologist in one city can contour structures, while a physicist in another can plan the dose, all using shared DICOM files. This is particularly beneficial in multidisciplinary tumor boards and healthcare settings with limited on-site expertise.
Platforms like PostDICOM take these advantages further by offering cloud-based DICOM viewing and collaboration tools. With PostDICOM, healthcare teams can upload, view, annotate, and share radiation therapy files in real time. This means faster turnaround times, reduced errors, and a more streamlined patient care process.
Radiation therapy is a powerful treatment modality, but its success hinges on accuracy and careful planning. From the initial CT or MRI scan to the complex algorithms defining dose delivery, every step relies on precise imaging data. DICOM makes this precision possible. It connects machines, professionals, and workflows into a cohesive system that prioritizes patient safety and treatment efficacy.
Understanding how radiation planning works with DICOM images is essential for anyone involved in oncology or radiology. It demystifies the behind-the-scenes work that turns abstract scans into actionable treatment plans.
Whether you're a professional exploring advanced tools or an institution seeking a better way to manage medical imaging, PostDICOM offers a robust solution. Try a free trial of PostDICOM today and experience the future of cloud-based radiotherapy imaging and planning.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |