
Blood clots can be silent killers. When they form in blood vessels, they have the potential to restrict or completely block blood flow, leading to serious complications such as deep vein thrombosis (DVT), pulmonary embolism (PE), stroke, or heart attack. The danger of clots lies in their unpredictability and speed. A clot dislodged from the leg can travel to the lungs and cause a potentially fatal embolism in mere seconds. For clinicians, detecting these clots quickly and accurately is not just beneficial—it's essential.
Medical imaging plays a pivotal role in this process. While traditional diagnostic methods such as physical exams and blood tests can suggest the presence of a clot, they do not confirm its location or severity. Imaging is the key to seeing inside the body in real-time, visualizing blood flow, and identifying clot formation. Among the many imaging options available today, Magnetic Resonance Imaging (MRI) stands out as a powerful, non-invasive, and radiation-free tool. But can MRI actually see blood clots? That’s the central question this article explores.
We’ll dive deep into how MRI visualizes clots, how it compares to other imaging options like CT and ultrasound, what types of vascular conditions it can detect, and when MRI is the best choice. If you're a radiologist, medical student, or a clinician making imaging decisions, understanding how MRI handles clot detection can enhance diagnostic precision and potentially save lives.
Yes, blood clots can show up in MRI scans, but it depends on several factors, including the age of the clot, its location, and the specific MRI technique used. MRI is especially effective in detecting clots in the brain, spine, pelvis, and deep veins that may be difficult to visualize with other methods.
MRI uses powerful magnetic fields and radio waves to generate detailed images of soft tissues. When it comes to blood clots, specialized forms of MRI, such as Magnetic Resonance Venography (MRV) or contrast-enhanced MRI, are used to visualize venous structures and vascular flow. These techniques can detect clots by identifying areas where blood flow is obstructed or abnormal signal intensities suggest thrombus formation.
Clots appear differently on MRI depending on their stage. Fresh clots appear isointense or slightly hyperintense on T1-weighted images and hypointense on T2-weighted images. These signals shift as the clot matures and undergoes chemical changes, allowing radiologists to estimate clot age and consistency.
One of the clearest examples of MRI's effectiveness is in detecting cerebral venous sinus thrombosis (CVST), a condition where clots form in the veins that drain blood from the brain. In such cases, MRI combined with MRV is considered the gold standard because of its ability to detect even subtle abnormalities in venous drainage patterns.
While not always the first-line imaging method for all types of clots, MRI provides unparalleled detail in specific clinical situations and body regions where other modalities may fall short.
The answer to this question is situational and depends on the suspected location of the clot, the urgency of the situation, and the patient's health background. No single scan is universally the "best," but rather each imaging modality serves a distinct purpose.
For example, ultrasound is widely used and often the first imaging technique chosen for detecting deep vein thrombosis (DVT) in the legs. It is non-invasive, affordable, and provides real-time evaluation of blood flow in superficial and deep veins. However, ultrasound's effectiveness is limited in obese patients, pelvic veins, and some central vessels.
In contrast, CT angiography (CTA) is usually the go-to for suspected pulmonary embolism due to its speed, wide availability, and high-resolution visualization of pulmonary arteries. CTA can clearly reveal clots blocking major vessels in the lungs and is often used in emergency settings.
MRI, however, is particularly advantageous in detecting clots in areas where ultrasound and CT may not be as effective or when radiation exposure is a concern. For example, pelvic vein thrombosis, spinal venous occlusions, and cerebral venous clots are best visualized with MRI. It is also preferred in younger patients and pregnant women where radiation should be avoided.
So while MRI might not always be the first scan ordered, it is often the most informative for complex or less accessible vascular regions. In combination with the right protocols and contrast agents, MRI becomes a powerful diagnostic ally.
MRI is not just limited to detecting thrombi; it is a versatile tool that can evaluate a wide range of blood-related conditions. For instance, vascular inflammation (vasculitis), aneurysms, and arteriovenous malformations (AVMs) can be assessed using MR angiography. This technique allows for a detailed visualization of blood vessel anatomy without requiring the use of ionizing radiation.
MRI can also identify hemorrhages, particularly in the brain, where the magnetic properties of blood products change depending on the stage of bleeding. These changes produce characteristic signal alterations on T1- and T2-weighted sequences, helping clinicians determine the age of a hemorrhage.
In more advanced settings, functional MRI (fMRI) and perfusion MRI techniques are used to assess blood flow and oxygenation in tissues. These are particularly helpful in stroke management, tumor grading, and evaluating tissue viability.
Blood-related problems such as iron overload disorders (hemochromatosis), bone marrow disorders, and even sickle cell disease can also show up in MRI scans through indirect markers like altered marrow signal or vascular changes.
In short, MRI is a powerful tool that extends well beyond clot detection. Its ability to image soft tissues with high resolution and without radiation makes it indispensable in evaluating a broad spectrum of hematologic and vascular conditions.
Despite its many strengths, MRI is not without limitations. One of the primary challenges is availability. MRI machines are not as widely available as CT scanners, especially in smaller hospitals or developing regions. Scanning times are also longer, which may not be ideal in emergency scenarios where rapid diagnosis is critical.
Cost is another significant factor. MRI exams tend to be more expensive than ultrasound or CT, which can limit their use in routine diagnostics unless absolutely necessary.
Additionally, contraindications exist for certain patients. Those with pacemakers, cochlear implants, or certain types of metal in their body may not be eligible for MRI due to safety concerns. Claustrophobic patients may also find the procedure uncomfortable, although open MRI systems are mitigating this issue.
There are also technical limitations in visualizing small, acute clots without the use of contrast agents. In some cases, MRI may fail to detect newly formed or minute thrombi, especially in areas with low signal contrast or movement artifacts.
Given these factors, while MRI is excellent for certain types of clots and body areas, it is often used in conjunction with other imaging modalities or reserved for cases that require additional detail.
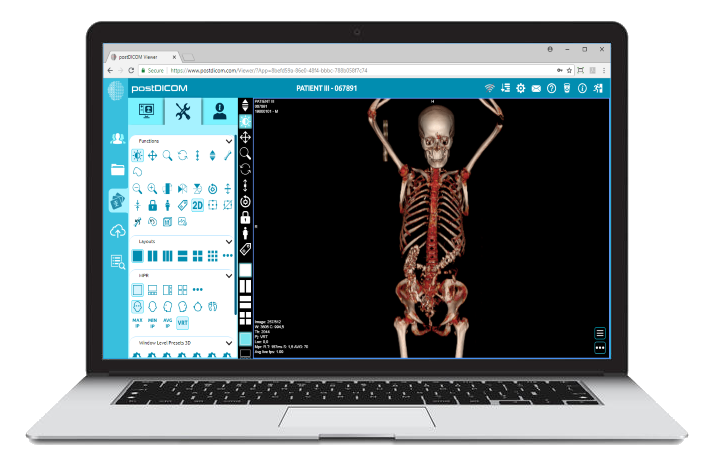
 - Created by PostDICOM.jpg)
MRI is not always the first imaging choice, but there are specific scenarios where it is the best or only viable option. One key example is cerebral venous sinus thrombosis (CVST), where MRI combined with MRV provides unmatched visualization of the cerebral venous system.
Another scenario involves pelvic vein thrombosis, which can be difficult to detect using ultrasound. MRI can penetrate deeper tissues and provide a more accurate assessment, making it useful for patients with unexplained pelvic pain or suspected venous obstruction.
Spinal venous thrombosis, although rare, is best diagnosed with MRI due to the complexity of spinal anatomy and the need for detailed imaging.
MRI is also ideal for young patients, pregnant women, or those who need frequent imaging, as it avoids radiation exposure. In such cases, MRI becomes not only a diagnostic tool but a safer long-term monitoring option.
Finally, MRI should be considered when other imaging modalities fail to provide a conclusive diagnosis. If a patient continues to show symptoms of a clot but has negative ultrasound or CT results, MRI can serve as a tiebreaker that leads to accurate diagnosis and appropriate treatment.
So, can MRI see blood clots? The answer is a definitive yes—and not only that, it can often see what other scans miss. MRI's versatility, depth of imaging, and ability to visualize complex vascular territories make it a critical tool in the diagnostic arsenal. While it may not always be the first option due to cost, time, or availability, it shines in cases that require detail, precision, and safety.
From detecting cerebral and pelvic clots to identifying vascular abnormalities and blood flow problems, MRI plays an expanding role in modern vascular imaging. For radiologists and clinicians looking to improve diagnostic accuracy, MRI offers a powerful advantage.
Platforms like PostDICOM further enhance this power by offering cloud-based tools that let you store, share, and analyze MRI scans with ease. Whether you’re collaborating across locations or archiving cases for research, PostDICOM ensures that your vascular imaging data is accessible, secure, and easy to navigate.
Ready to elevate your imaging workflow? Try PostDICOM for free today and experience the next level of medical image management.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |