In recent years, artificial intelligence has revolutionized numerous sectors, and healthcare is no exception. Within the realm of medical imaging, AI has emerged as a powerful tool that is reshaping how radiologists work, improving diagnostic accuracy, and enhancing patient care. This blog explores the multifaceted role of AI in radiology, its historical development, and its promising future applications.
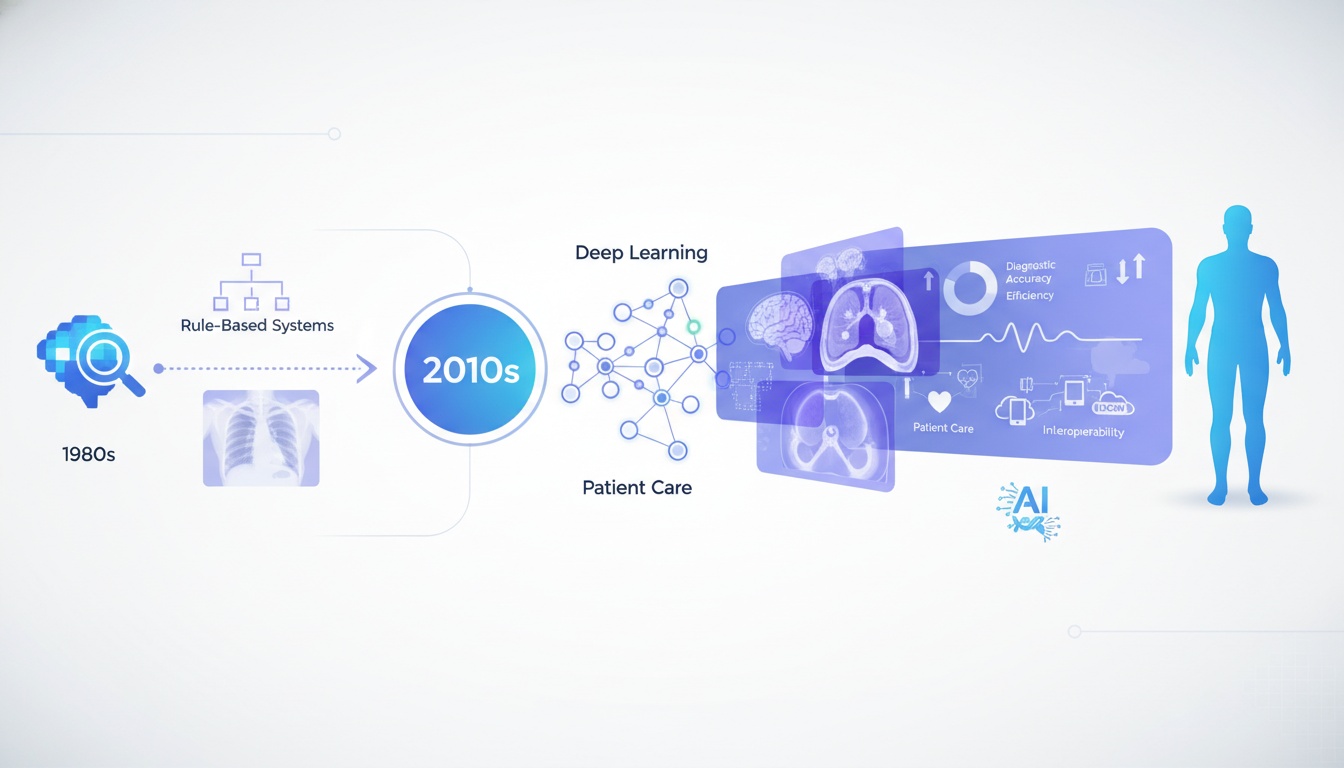
The journey of AI in radiology began in the late 1980s with rule-based expert systems designed to detect simple abnormalities. However, these early systems lacked the sophistication needed for clinical application. The true breakthrough came in the 2010s with the advent of deep learning, a subset of machine learning based on artificial neural networks.
In 2012, the ImageNet competition demonstrated the extraordinary potential of convolutional neural networks (CNNs) for image recognition. By 2015, researchers began applying similar deep learning techniques to medical imaging, marking the beginning of the modern era of AI in radiology.
Today, AI algorithms can analyze medical images with remarkable accuracy, sometimes matching or even surpassing human performance in specific tasks. The FDA has approved numerous AI-based medical imaging tools since 2017, indicating the maturity and reliability of these technologies.
AI integration in radiology encompasses several levels of technological implementation, from basic image enhancement to complex diagnostic decision support systems. Here's how AI is being integrated into the radiological workflow:
1. Image Acquisition and Enhancement
AI algorithms can optimize scan parameters in real-time, reducing radiation exposure while maintaining image quality. They can also enhance image clarity by reducing noise, improving contrast, and correcting artifacts, enabling radiologists to identify subtle abnormalities more easily.
2. Image Interpretation and Analysis
This represents the most visible application of AI in radiology. Deep learning models can detect, characterize, and quantify abnormalities across various imaging modalities, including:
• X-rays: Detecting lung nodules, pneumonia, tuberculosis, and fractures
• Ct Scans: Identifying stroke, pulmonary embolism, coronary artery disease, and cancer
• Mri: Analyzing brain tumors, multiple sclerosis lesions, and musculoskeletal disorders
• Mammography: Detecting and classifying breast lesions
3. Workflow Optimization
AI can prioritize critical cases in radiologists' worklists, ensuring that life-threatening conditions receive immediate attention. Additionally, automated report generation tools can draft preliminary findings, allowing radiologists to focus on interpretation rather than documentation.
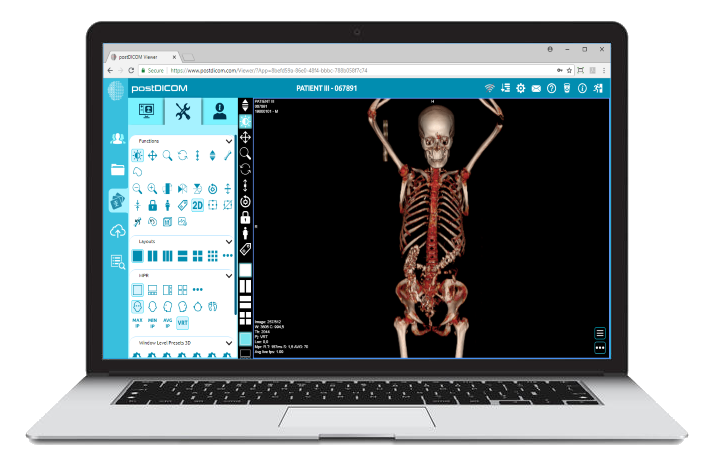
4. Integration with Cloud PACS Systems
Modern cloud-based Picture Archiving and Communication Systems (PACS) like PostDICOM are embracing AI integration. These systems leverage cloud technologies to provide the scalable storage and processing power necessary for AI algorithms. PostDICOM, for instance, offers a comprehensive solution that combines cloud PACS with advanced diagnostic tools and teaching capabilities.
The integration of AI with cloud PACS enables:
• Seamless Access To Ai Analysis Tools Within The Standard Workflow
• Real-time Collaboration Between Ai Algorithms And Radiologists
• Continuous Learning And Improvement Of Ai Models Through Access To Larger Datasets
• Remote Access To Both Images And Ai-assisted Interpretations
Beyond diagnostic radiology, AI is making significant inroads into radiation oncology, transforming how cancer patients receive treatment:
1. Treatment Planning
AI algorithms can automatically segment tumors and organs at risk (OARs) on planning CT scans—a task that traditionally requires hours of manual contouring by radiation oncologists. This not only saves time but also improves consistency across different practitioners.
AI can also generate optimal radiation treatment plans by analyzing thousands of previous cases, taking into account tumor characteristics, patient anatomy, and desired outcomes. These AI-generated plans often achieve better dose distributions than manually created ones, sparing healthy tissues while ensuring adequate target volume coverage.
2. Adaptive Radiotherapy
Tumors and surrounding anatomy can change during radiation therapy due to tumor shrinkage, weight loss, or organ movement. AI enables real-time monitoring of these changes through daily imaging, allowing for prompt adjustments to the treatment plan. This "adaptive radiotherapy" approach ensures that radiation is always precisely targeted at the tumor, even as its location and shape evolve.
3. Response Prediction and Monitoring
AI algorithms can analyze pre-treatment images to predict which patients will respond well to radiation therapy, helping clinicians select the most appropriate treatment approach for each individual. During and after treatment, AI can detect subtle signs of response or recurrence that might be missed by human observers, enabling earlier intervention when necessary.
Interventional radiology involves minimally invasive image-guided procedures to diagnose and treat diseases. AI is enhancing this field in several ways:
1. Procedure Planning and Navigation
AI algorithms can analyze pre-procedural images to identify optimal approaches for biopsies, ablations, and other interventions. During procedures, AI-enhanced navigation systems can guide instruments precisely to their targets while avoiding critical structures, even compensating for patient movement and breathing.
2. Real-time Decision Support
Interventional procedures often require rapid decision-making based on fluoroscopic or ultrasound images. AI can provide real-time analysis of these images, highlighting relevant anatomical structures, flagging potential complications, and suggesting corrective actions.
3. Outcome Prediction
By analyzing patient characteristics and procedural details, AI models can predict the likelihood of technical success, clinical improvement, and potential complications. This information helps interventional radiologists select the most appropriate candidates for specific procedures and prepare for possible challenges.
 - Created by PostDICOM.jpg)
1. Improved Diagnostic Accuracy
AI systems excel at pattern recognition and can detect subtle abnormalities that might be overlooked by human observers, particularly when radiologists are fatigued or working under time pressure. Recent studies have determined that AI-assisted mammography can reduce false-positive biopsy rates by 69%.
2. Enhanced Efficiency
With radiologists facing increasing workloads, AI can handle routine cases or preliminary screenings, allowing human experts to focus on complex cases requiring their specialized knowledge. This workflow optimization can reduce reporting times and help address the global shortage of radiologists.
3. Quantitative Analysis
Unlike human observers, AI systems can provide precise measurements and quantitative assessments of imaging findings, enabling more objective monitoring of disease progression and treatment response.
4. Accessibility
Cloud-based AI solutions like those integrated with PostDICOM democratize access to expert-level image analysis, bringing advanced diagnostic capabilities to underserved regions and smaller healthcare facilities.
1. Data Quality and Bias
AI algorithms are only as good as the data they're trained on. Models developed using data from specific populations or imaging equipment may not perform well in different settings. Ensuring diverse, representative training data is essential to avoid perpetuating or amplifying existing healthcare disparities.
2. Interpretability and Trust
Many deep learning models operate as "black boxes," making it difficult for radiologists to understand how they arrive at specific conclusions. Developing explainable AI systems is crucial for building trust among healthcare professionals and ensuring responsible clinical implementation.
3. Regulatory and Ethical Considerations
Questions about liability, patient consent, and privacy become increasingly complex as AI systems take on greater roles in medical decision-making. Clear regulatory frameworks and ethical guidelines are needed to address these concerns.
The future of AI in radiology lies not in replacing radiologists but in creating powerful synergies between human expertise and machine intelligence. We are moving toward a model of "augmented radiology," where AI handles routine tasks, detects subtle abnormalities, and provides quantitative analyses, while radiologists focus on complex interpretations, integration of clinical information, and direct patient care.
Emerging technologies like federated learning will enable AI models to learn from data across multiple institutions without compromising privacy, accelerating development while addressing concerns about data sharing. Meanwhile, multimodal AI systems will integrate information from diverse sources—imaging, electronic health records, genomics, and wearable devices—to provide comprehensive assessments of patient health.
AI is transforming radiology from a primarily interpretive specialty to a data-driven discipline capable of extracting unprecedented insights from medical images. From streamlining workflows to improving diagnostic accuracy and personalizing treatment plans, AI tools are enhancing radiologists' capabilities across the board.
Solutions like PostDICOM exemplify this evolution, combining cloud-based PACS with advanced diagnostic tools and AI integration to offer a comprehensive platform for modern radiology practice. With features like MPR, MIP, and 3D rendering alongside seamless sharing capabilities, such systems represent the future of radiological practice.
As we navigate this exciting technological frontier, the focus must remain on developing AI tools that augment human expertise rather than replace it, ensuring that these powerful technologies serve their ultimate purpose: improving patient outcomes through better, faster, and more accessible diagnostic imaging.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |