
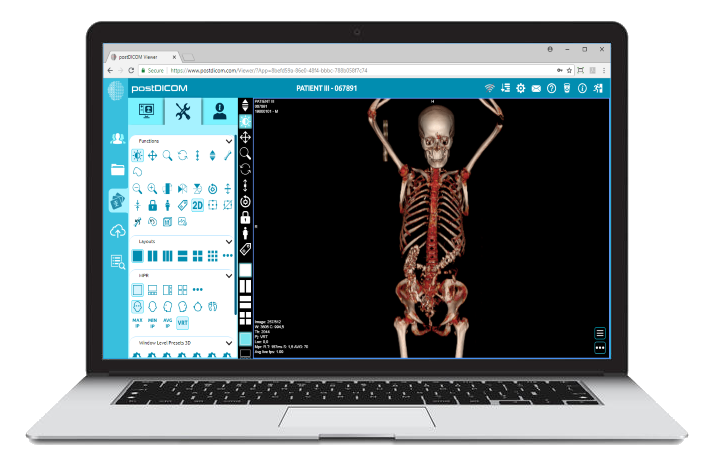
In the bustling corridors of a modern hospital, a radiologist pulls up a patient's MRI on a state-of-the-art DICOM viewer. A few floors above, a surgeon accesses the same patient's previous X-rays on a different system.
Armed with cutting-edge technology, both medical professionals are poised to deliver exceptional care. But there's a catch: the two systems struggle to communicate seamlessly despite housing the same type of data.
This scenario, unfortunately, isn't a rare anomaly but a reflection of a widespread challenge in the world of medical imaging: interoperability.
In an era where technology promises boundless integration, the medical community often grapples with the reality that not all DICOM systems and viewers are created equal—or compatible.
Join us on this journey as we navigate the complexities of ensuring that different DICOM platforms speak the same language and understand each other perfectly.
Interoperability, at its core, refers to the ability of different information systems, devices, or applications to connect, communicate, and work together cohesively.
In medical imaging, this means that DICOM viewers, storage systems, and other related platforms should be able to exchange and interpret shared data without hitches.
The bridge ensures that a patient's imaging data is accessible, consistent, and usable across various platforms and institutions.
The significance of interoperability extends far beyond mere technical integration. For medical professionals, it's about having timely access to comprehensive patient data, irrespective of where or how it was acquired.
This seamless flow of information is crucial for accurate diagnoses, informed decision-making, and effective treatments. In essence, interoperability directly impacts the quality and efficiency of patient care, ensuring that medical histories are not fragmented but unified narratives guiding healthcare journeys.
The DICOM (Digital Imaging and Communications in Medicine) standard was introduced in the 1980s to respond to the growing need for a universal format for medical images.
Over the years, as medical imaging technologies evolved, so did the DICOM standard, expanding its scope and refining its specifications. However, despite a standardized protocol, variations in implementation and the introduction of proprietary extensions by different vendors have posed challenges.
The very standard designed to unify has sometimes been a source of divergence, underscoring the complexities of achieving true interoperability.
At first glance, adhering to the DICOM standard would ensure flawless communication between systems.
However, the reality is more intricate. In their quest to offer unique features or optimize performance, different vendors might introduce variations in their DICOM implementations. These subtle differences, while often well-intentioned, can lead to compatibility issues.
For instance, how one system encodes or compresses an image might not be seamlessly decoded by another, leading to data loss or misinterpretation.
Beyond the technical realm, organizational challenges are significant in interoperability issues. Medical institutions might operate on legacy systems and be reluctant to upgrade due to costs or potential disruptions.
These older systems, while functional, might not be equipped to communicate with newer, more advanced platforms.
Additionally, in an attempt to create a unique market niche, some vendors develop proprietary extensions or features that aren't universally supported. This creates silos, where data within one system remains trapped and inaccessible to others.
 - Created by PostDICOM.jpg)
Even when systems are technically capable of communicating, data-related challenges can arise. Inconsistencies in data formats, variations in metadata tagging, or even differences in how patient information is recorded can hinder seamless data exchange.
For instance, a CT scan labeled with a specific patient identifier in one system might not match the identifier used in another, leading to potential mismatches or data duplication.
While seemingly minor, these discrepancies can have significant implications, especially when accurate patient data is paramount for diagnostics and treatments.
The potential delay in patient care is the most immediate and concerning consequence of limited interoperability. When medical professionals cannot access or integrate essential imaging data promptly, it can delay diagnosis, treatment planning, or surgical interventions.
In critical situations, where time is of the essence, such delays can have dire consequences. Moreover, manually transferring or converting data can introduce errors, further complicating the patient care process.
Beyond the clinical implications, limited interoperability carries significant financial costs. Institutions may invest in additional software or hardware to bridge compatibility gaps.
While seemingly straightforward, manual data transfers or conversions require time and resources, leading to increased operational costs.
Furthermore, data discrepancies or errors arising from interoperability issues can lead to billing inaccuracies, claim denials, or potential legal ramifications.
At the heart of medical care lies the oath to do no harm. However, limited interoperability can inadvertently introduce risks to patient safety. Misaligned or mismatched data can lead to incorrect diagnoses or inappropriate treatments.
Additionally, the integrity of medical data is paramount. With interoperability challenges, data corruption, loss, or unauthorized access is risky during transfers or conversions.
A pressing concern is ensuring that patient data remains accurate, complete, and secure amidst these challenges.
One of the most fundamental solutions to address interoperability challenges is the strict adherence to standardized protocols. Many technical compatibility issues can be mitigated by ensuring that DICOM implementations align with universally accepted standards.
Regular audits, validations, and conformance testing can ensure that systems remain compliant and interoperable. Institutions and vendors must prioritize and champion these standards, recognizing them as the bedrock of seamless communication.
The rise of Vendor-Neutral Archives (VNAs) and universal viewers offers a promising solution to interoperability woes. VNAs allow medical institutions to store imaging data in a standardized format, regardless of source or system.
This centralization ensures that data remains accessible and consistent across platforms. Universal viewers complement VNAs by providing a consistent viewing experience, regardless of the underlying data source or format.
Together, VNAs and universal viewers break down proprietary barriers, fostering a more integrated and collaborative imaging environment.
Interoperability isn't just a technical challenge; it's a collective one. Industry consortiums, open-source initiatives, and global standardization drives are pivotal in addressing interoperability issues.
By fostering collaboration between vendors, medical institutions, and professionals, these collective efforts work towards creating universally accepted standards, best practices, and solutions.
Sharing knowledge, experiences, and challenges within these collaborative platforms accelerates the journey towards genuine interoperability.
Across the globe, many institutions have successfully navigated interoperability challenges, offering valuable insights and lessons.
For instance, a multi-hospital network in Scandinavia implemented a unified VNA, streamlining data access across facilities and enhancing patient care continuity.
Another success story comes from a radiology clinic in North America that adopted a universal viewer, simplifying workflows and reducing training needs. These real-world implementations underscore the tangible benefits of prioritizing interoperability and offer a roadmap for others to follow.
The intricate dance of DICOM systems, with their myriad of viewers, platforms, and data formats, paints a picture of a medical imaging landscape rich in potential yet riddled with challenges.
As we've journeyed through the complexities of interoperability, it's evident that seamless communication is more than a technical aspiration; it's a cornerstone of optimal patient care, efficient workflows, and financial prudence.
While the road to true interoperability is paved with obstacles, the combined forces of standardized protocols, innovative solutions, and collective action shine a beacon of hope.
As we stand at this crossroads, one thing is clear: the future of DICOM, driven by collaboration and innovation, promises a harmonious symphony where every system, viewer, and data point plays in perfect tune.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |