
Chronic diseases continue to impose an increasing burden on North American healthcare. Effectively managing these persistent conditions is a complex challenge, requiring regular monitoring, personalized care, and efficient health information exchange.
This is where Electronic Health Records (EHRs) can revolutionize the game. EHRs empower healthcare providers with the right tools to tackle chronic disease management head-on by providing an innovative platform to unify patient data.
In this blog post, we delve into how EHRs can transform chronic disease management, enhance patient outcomes, and streamline healthcare delivery, thus genuinely becoming a game changer in modern healthcare.
Electronic Health Records (EHRs) are digital versions of a patient's medical history maintained over time by healthcare providers. Unlike traditional paper-based records, EHRs are dynamic and interactive, capable of aggregating information from multiple sources, including doctors, specialists, and labs.
These systems house a wealth of information, from demographic data to clinical histories, laboratory results, medications, and more. But EHRs are not just digital filing cabinets; they're intelligent platforms that can analyze data, send reminders for preventive screenings, and flag potential medical issues.
This combination of comprehensive data gathering and intelligent features positions EHRs as powerful tools in managing healthcare, including chronic diseases, which we'll explore in future sections.
Chronic diseases such as heart disease, diabetes, and respiratory illnesses have become a significant public health concern in North America, affecting nearly half the adult population.
These conditions compromise the quality of life and burden the healthcare system, accounting for a significant proportion of healthcare spending.
In the face of this chronic disease epidemic, effective and efficient management strategies are more critical than ever. Traditional methods of disease management are often reactive and fragmented, leading to suboptimal patient outcomes and higher healthcare costs.
However, integrating modern technology, such as Electronic Health Records (EHRs), into disease management holds immense potential to address these challenges and transform the landscape of chronic disease management.
EHRs are becoming increasingly instrumental in chronic disease management, providing various features and capabilities that enable patients and healthcare providers to monitor and manage chronic conditions more effectively.
One of the standout features of EHRs is the patient portal, an interface that allows patients to access their health records, view lab results, schedule appointments, and communicate with their doctors securely.
This empowers patients to be more engaged in their care, a critical aspect of managing chronic conditions that often require significant lifestyle changes and regular treatment adherence.
Moreover, EHRs can facilitate the tracking of medications, reducing errors and ensuring that patients adhere to their prescribed treatments. This is crucial in chronic disease management, where patients must take multiple medications over long periods.
EHRs can even send reminders to patients to take their medications, increasing adherence rates.
EHRs also offer clinical decision support systems (CDSS). These intelligent tools can analyze patient data and alert healthcare providers when a patient's condition deviates from expected outcomes or when preventive measures are due.
This proactive approach is particularly beneficial in managing chronic diseases, where early intervention can prevent complications and improve patient outcomes.
Health analytics is another critical component of EHRs. With the ability to analyze large volumes of data, EHRs can help identify trends and patterns in a patient's condition.
For instance, a healthcare provider can monitor blood sugar levels in a diabetic patient over time, identifying trends that may indicate the need for treatment adjustments.
Further, EHRs facilitate better coordination of care. In managing chronic diseases, a patient often needs to see multiple specialists.
EHRs enable seamless information exchange between healthcare providers, ensuring every provider can access the most current and comprehensive patient information. This can lead to more accurate diagnoses, targeted treatments, and better patient outcomes.
A notable example of EHRs' impact on chronic disease management is seen in a study by Kaiser Permanente. The study found that implementing an EHR-based system led to significant improvements in drug treatment intensification, monitoring, and risk factor control among patients with diabetes.
EHRs are revolutionizing chronic disease management through these features, offering tools and resources that make care more proactive, personalized, and effective.
The adoption of EHRs in chronic disease management brings significant benefits to both patients and healthcare providers, as well as the healthcare system as a whole.
EHRs can significantly enhance patient outcomes by promoting proactive, personalized care. With the ability to monitor patient data over time and alert providers to potential issues, EHRs can help catch complications early and prevent adverse health events.
The interactive nature of EHRs also encourages patients to take an active role in their health, which has been shown to improve outcomes in chronic disease management.
Managing chronic diseases often involves multiple healthcare providers from various specialties. EHRs allow for seamless information sharing across providers, ensuring everyone involved in a patient's care can access up-to-date, comprehensive information.
This enhances care coordination, reduces the risk of medical errors, and helps ensure patients receive the most appropriate treatments.
By promoting preventive care, improving coordination, and minimizing errors, EHRs can lead to considerable cost savings. Studies have shown that EHRs can reduce the number of duplicate tests and preventable hospitalizations, significantly reducing healthcare costs.
Furthermore, EHRs can improve efficiency by automating administrative tasks, freeing time for healthcare providers to focus on patient care.
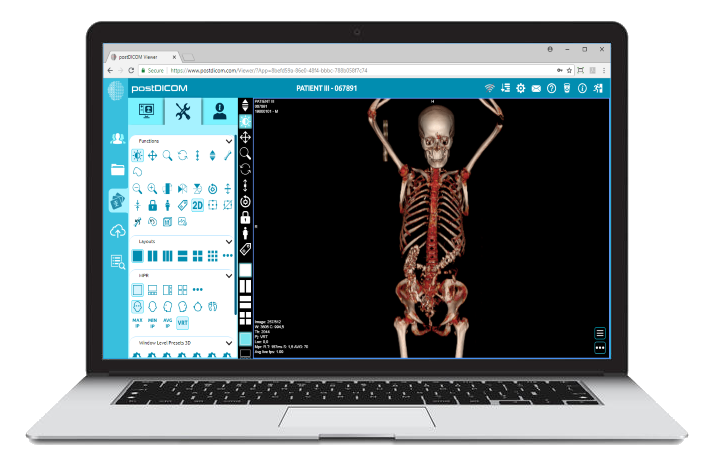
 - Created by PostDICOM.jpg)
EHRs offer patient portals, allowing patients to access their medical records, communicate with their providers, and manage their appointments. This level of access and transparency promotes patient engagement, a critical factor in managing chronic diseases.
When patients are actively involved in their care, they are more likely to adhere to treatment plans and make lifestyle changes to improve their health.
EHRs gather a wealth of data that can be used for research purposes and population health management.
This data can provide insights into the prevalence and management of chronic diseases in different populations, helping public health officials develop targeted interventions and policies.
While the benefits of EHRs in chronic disease management are compelling, there are challenges that healthcare providers may encounter during their implementation and use. Recognizing these challenges and understanding how to overcome them is crucial for leveraging EHRs effectively.
The initial cost of purchasing and implementing an EHR system and ongoing maintenance and update costs can be significant. However, numerous government incentives, such as the Promoting Interoperability Programs in the U.S., are designed to help healthcare providers offset these costs.
The long-term savings from improved efficiency and reduced healthcare costs can also outweigh the initial investment.
The digital nature of EHRs raises concerns about the privacy and security of sensitive patient information.
Healthcare providers must choose EHR systems that comply with relevant regulations such as HIPAA in the U.S. Regular staff training on privacy practices and investment in secure IT infrastructure can also help mitigate these concerns.
Healthcare providers may resist transitioning to EHRs due to a lack of familiarity with technology or fear of change.
Overcoming this resistance involves providing comprehensive training, ensuring user-friendly design, and demonstrating the benefits of EHRs for patients and healthcare providers.
While EHRs facilitate seamless information exchange, interoperability can be challenging when healthcare providers use different EHR systems.
This has been a significant focus of current healthcare IT standards and policies, and providers are encouraged to choose EHR systems that adhere to these standards.
EHRs present a transformative solution to managing the chronic disease epidemic in North America. Their various features – from patient portals to health analytics and care coordination – empower healthcare providers to offer personalized, proactive care.
While the implementation of EHRs presents some challenges, the strategic deployment and use of these systems, with appropriate support and planning, can overcome these hurdles. The potential benefits, from improved patient outcomes to reduced healthcare costs, affirm the game-changing role of EHRs in modern healthcare.
As we continue to innovate, EHRs will undoubtedly play an increasingly pivotal role in shaping the future of chronic disease management.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |